CT SCAN
Computed Tomography (CT)
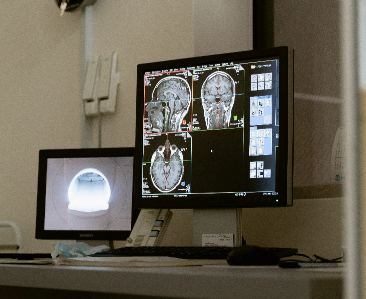
Computed tomography (CT) imaging, also known as "CAT scanning" (Computerized Axial Tomography), provides a different form of imaging known as cross-sectional imaging. The origin of the word "tomography" is from the Greek word "tomos" meaning "slice" or "section" and "graphe" meaning "drawing." A CT imaging system produces cross-sectional images or "slices" of anatomy, like the slices in a loaf of bread.
Computed Tomography (CT) has witnessed a change over the past 20 years. It is said that the use of CT for applications in radiological diagnosis during the 70s sparked a revolution in the field of medical engineering. Innovative scanners, advanced applications were introduced in the CT technology that brought about exciting breakthroughs in clinical procedures that helped in addressing various public health issues. In the Indian scenario, CT technology has today become an indispensable and integral component of routine work in clinical and medical practice, specifically in radio-diagnosis and procedures such as colonography, cancer detection and staging, lung analysis, angiographic studies and radiotherapy planning
(32 slices/sec reconstruction)
1st Prestigious Installation of 32 Slices CT by Siemens Go Now in Uttarakhand(Introduced in 2017 worldwide).
Salient Features:
*Excellent spatial & temporal resolution.
*Reduced scan time.
*Isotropic imaging possible.
*Better multiplanar reconstructions.
*Virtual Bronchoscopy.
*Virtual Colonoscopy.
*Excellent Contrast Angiography.
*Slices as thin as 0.625 mm possible.
*3D reconstruction of inner joint.
*Multiphase CT for Liver, Pancreas & Kidneys.
CT Preparation Instructions
General Instructions
Wear comfortable clothing free of zippers, metallic buttons as well as jewellery that could interfere with your scan. Elastic Waist Bands and Sport Bras are acceptable.
Please notify the doctor if you have any allergy to iodine or intravenous contrast, if so you need to be pre-medicated.
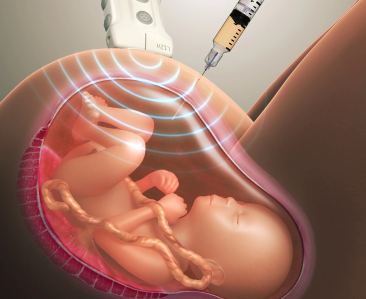
Female patients must notify if they are or think they might be pregnant, for further instructions.
A blood test (Creatinine) is required within 6 weeks of CT examinations ordered with IV Contrast.
Patient Screening Prior to Administration of Iodinated Contrast
Prior to the administration of iodinated contrast, patients are screened for the following:
Previous reactions to iodinated contrast media
All severe allergies and reactions (both medications and food)
History of diabetes, kidney disease, pheochromocytoma, solitary kidney, kidney or other transplant, or myeloma
Current use of any containing medications
For women of child-bearing age, currently or possibly pregnant or currently breast-feeding.
Premedication Instructions for Patients with Contrast Allergies
Contrast Administration in Patients with Elevated Creatinine
Estimated glomerular filtration rate is a better predicator of renal dysfunction than creatinine alone. The decision to proceed with contrast administration in patients with an estimated GFR < 45 ml/min/1.732 is a matter of clinical judgment, based on the individual circumstances of the patient and following consultation between the radiologist and requesting physician. Strategies to prevent nephropathy in patients with renal impairment include hydration, reduction of contrast dose, and discontinuation of nephrotoxic drugs. A critical diagnostic study should not be delayed because of excessive concern regarding possible contrast nephropathy.
Contrast Administration in Patients with Renal Failure
Patients on dialysis can receive IV contrast, and early post-procedural dialysis is not routinely required; however, the fact that a patient is on dialysis should not be regarded as automatically allowing the administration IV contrast. The administration of contrast may jeopardize the return of renal function in patients who are receiving dialysis for acute renal failure and may further worsen renal function in patients who still make some urine but receive dialysis intermittently. The volume of iv contrast should also be considered in patients on dialysis who are at risk for volume overload.
Contrast Administration in Patients Receiving
Diabetic Patients: If you are a diabetic patient taking any medication that contains and are scheduled for an examination that requires IV contrast (CT, IVP) DO NOT take your medications on the day of your appointment and for 48 hours following completion of your imaging examination and reinstituted only after renal function has been re-evaluated and found to be normal.
Vascular Access and Use of Central Lines and Ports
IV Access for CT Studies
The type and location of intravenous access is determined by the examination to be performed.
A single-phase exam may be performed with hand injection via a 22G iv.
Multiphase exams and CT angiography can only be performed with pressure injector and a 20G iv or larger is required.
Right arm injection is preferred unless the exam is to evaluate the right upper arm arterial anatomy, in which case the left arm is used.
Pressure injector also is not permitted through an iv that is not functioning well, i.e. has poor blood return or is difficult or painful to flush.
Prepare a Patient for a CT
General Instructions
Little preparation is needed for a CT scan. Patients are asked to drink plenty of water both before and after the exam, especially if the exam is performed with oral or intravenous contrast. Patients will be asked to remove jewelry and other metallic objects that might interfere with the scan.
CT Imaging Examinations General Instructions The patient should have NOTHING to eat for 4 hours prior to a CT examination. Patients may only have clear liquids (water, apple juice). Patients should take their medications at the normal time with clear liquids only. Patients should not take the morning of the imaging study. Some patients may need to drink oral contrast. If the patient was dispensed oral contrast by the scheduling clinic, then the patient should drink the bottle 2 hours prior to their scheduled appointment. If the patient did not receive the contrast prior to his/her scheduled appointment time, then he/she must arrive in Radiology 2 hours prior to their examination time.
CT Examination of Head/Neck/Chest – with Contrast only (No special prep necessary without contrast) Nothing to eat or drink for 4 hours prior to the examination. If the patient has allergies to contrast, then the patient or relatives should inform the team beforehand. For diabetic patients having a CT examination with IV contrast, please see the instructions above. Take all non-diabetic medications as directed. CT Examination of Pelvis – With or Without Contrast Nothing to eat or drink for 4 hours prior to the examination. Drink first bottle of contrast 2 hours prior to the examination; drink the second bottle of contrast 60 minutes prior to the examination. If the patient has allergies to contrast, then the patient or relatives should inform the team beforehand. For diabetic patients having a CT examination with IV contrast, please see the instructions above. CT Examination Without Contrast No preparation is required.
FAQ'S
Q. What are the dangers of CT scanning?
Though it involves X-Ray radiations, there are no dangers in practice. Only for pregnant women, it should be done after weighing all the risks of exposing their fetus to radiations and benefits (like any other CT investigation). Dangers of contrast medium
Q. What is a 'contrast' medium?
A contrast is an iodinated compound injected intravenously (peripherally) to opacify the blood vessels and enhance the ability of CT scans to pick up abnormalities Only the very safest contrast (non-ionic) is used for all the patients in our centre. This gives better compliance with patients, as compared to ionic contrast, which is cheaper but, gives more adverse reactions.
* Dangers of contrast medium
* Though not so common, the contrast medium involved in a CT scan poses a slight risk of allergic reaction.
* Most reactions result in hives or itchiness.
* For individuals with asthma who become allergic to the contrast medium, the reaction can be an asthma attack
* In very rare instances, an allergic reaction might cause swelling in your throat or other areas of your body
* If you experience hives, itchiness or swelling in your throat during or after your CT exam, immediately tell your technologist or doctor. We keep an emergency kit for all commonly known adverse reactions.
Q. Who is at 'high-risk' for contrast injection?
* Past history of reaction to contrast/any other drugs.
* Bronchial asthma.
* Cardiac/kidney disease /diabetes etc.
Q. Other indications your doctor may recommend a CT scan to help?
* Diagnose muscle and bone disorders, such as bone tumors and fractures.
* Pinpoint the location of a tumor, infection or blood clot.
* Guide procedures such as surgery, biopsy and radiation.
* Detect and monitor diseases such as cancer.
* Detect internal injuries and internal bleeding.
Q. What can you expect during a CT scan?
During the CT scan, you lie on a narrow table that slides through the opening of a large device called the gantry. The table can be raised, lowered or tilted. Straps and pillows may help you stay in position. During a CT scan of the head, the table may be fitted with a special cradle that holds your head still.
As the X-Ray tube rotates around your body, the table slowly moves through the gantry. While the table is moving, you may need to hold your breath to avoid blurring the images. You may hear clicking and whirring noises. Each rotation yields several images of thin slices of your body.
During this time, a technologist in a shielded room supervises the CT scan and monitors the images as they appear on the computer screen. The technologist can see and hear you, and you can communicate via intercom.
If an infant or small child is having the CT scan, you may be allowed to stay with your child during the test. If so, you may be asked to wear a lead apron to shield you from X-ray exposure.
CT scans are painless. If your exam involves use of an intravenous contrast medium, you may feel a brief sensation of heat or experience a metallic taste in your mouth. If you receive contrast medium through an enema-to help highlight your lower gastrointestinal region-you may feel a sense of fullness or cramping.
After the exam, you can return to your normal routine. If you were given a contrast medium, your doctor or the radiography staff may give you special instructions. These likely include drinking lots of fluids to help remove the medium from your body.